Open Angle Glaucoma
It is estimated that over two million Americans have some type of glaucoma and half of them do not know it. Ninety percent of glaucoma patients have open angle glaucoma. Although it cannot be cured, it can usually be controlled. Vision loss may be minimized with early treatment. The eye receives its nourishment from a clear fluid that circulates inside the eye.
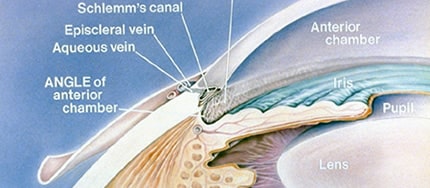
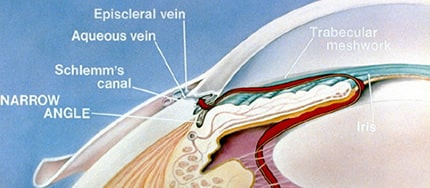
This fluid must be constantly returned to the blood stream through the eye’s drainage canal, called the trabecular meshwork. In the case of open angle glaucoma, something has gone wrong with the drainage canal. When the fluid cannot drain fast enough, pressure inside the eye begins to build.
This excess fluid pressure pushes against the delicate optic nerve that connects the eye to the brain. If the pressure remains too high for too long, irreversible vision loss can occur.
Fluid circulating inside eye
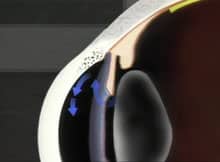
Excess fluid builds pressure
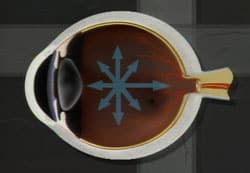
Excess fluid pressure pushes against the optic nerve
FAQ
Symptoms of Open Angle Glaucoma
- In the early stages, there are no symptoms. There is no pain or outward sign of trouble.
- Mild aching in the eyes
- Gradual loss of peripheral vision (the top, sides and bottom areas of vision)
- Seeing halos around lights
- Reduced visual acuity (especially at night, that is not correctable with glasses)
Who is at risk?
Glaucoma can occur in people of all races at any age. However, the likelihood of developing glaucoma increases if you;
- Are African American
- Have a relative with glaucoma
- Are diabetic
- Are very nearsighted
- Are over 35 years of age
Diagnosing Open-Angle Glaucoma
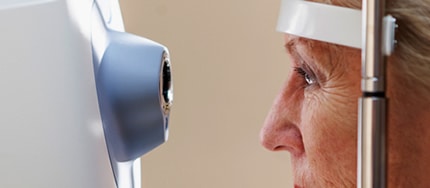
Everyone should be checked for glaucoma at around age 35 and again at age 40. Those considered to be at higher risk, including those over the age of 60 should have their pressure checked every year or two. Your doctor will use tonometry to check your eye pressure. After applying numbing drops, the tonometer is gently pressed against the eye and its resistance is measured and recorded.
An ophthalmoscope can be used to examine the shape and color of your optic nerve. The ophthalmoscope magnifies and lights up the inside of the eye. If the optic nerve appears to be cupped or is not a healthy pink color, additional tests will be run.
Perimetry is a test that maps the field of vision. Looking straight ahead into a white, bowl-shaped area, you’ll indicate when you’re able to detect lights as they are brought into your field of vision. This map allows your doctor to see any pattern of visual changes caused by the early stages of glaucoma.
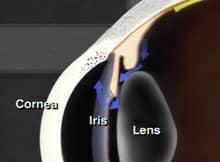
Gonioscopy is used to check whether the angle where the iris meets the cornea is open or closed. This helps your doctor determine if they are dealing with open-angle glaucoma or narrow-angle glaucoma.
Treatments for Open-Angle Glaucoma
To control glaucoma, your doctor will use one of three basic types of treatment: medicines, laser surgery, or filtration surgery. The goal of treatment is to lower the pressure in the eye.
Medicines
Medicines come in pill and eye drop form. They work by either slowing the production of fluid within the eye or by improving the flow through the drainage meshwork. To be effective, most glaucoma medications must be taken between one to four times every day, without fail. Some of these medications have some undesirable side effects, so your doctor will work with you to find a medication that controls your pressure with the least amount of side effects. Medicines should never be stopped without consulting your doctor, and you should notify all of your other doctors about the medications you are taking.
Argon Laser Trabeculoplasty
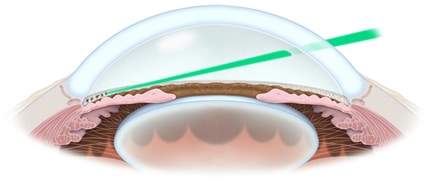
Argon Laser Trabeculoplasty and Selective Laser Trabeculoplasty surgery treat the drainage canal. Requiring only numbing eye drops, the laser beam is applied to the trabecular meshwork resulting in an improved rate of drainage. When laser surgery is successful, it may reduce the need for daily medications.
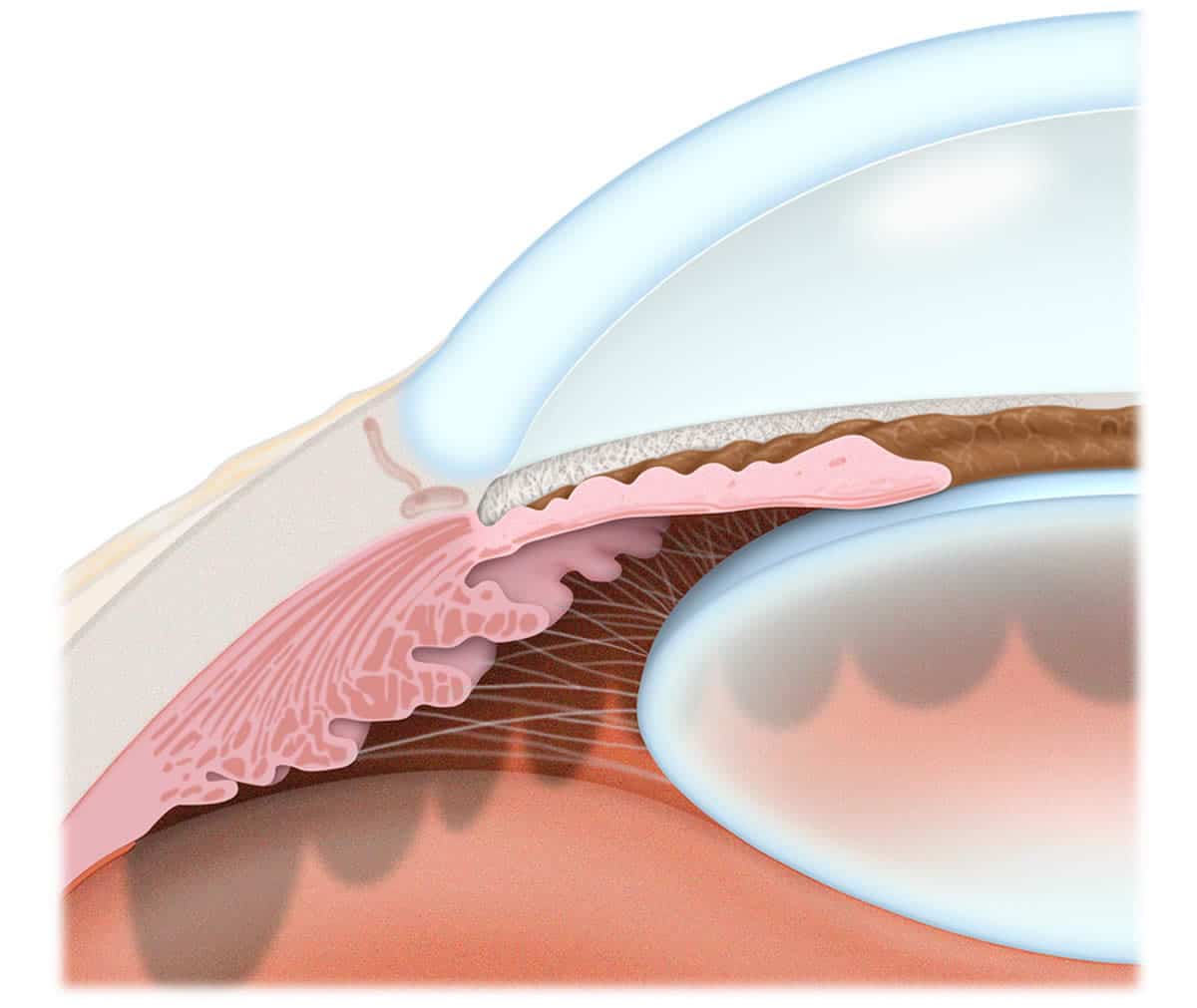
Endoscopic CycloPhotocoagulation (ECP)
Endoscopic CycloPhotocoagulation (ECP) is another type of laser procedure. Instead of treating the drainage canal, it treats the ciliary body. Treating the ciliary body reduces the amount of fluid production thereby reducing the intraocular pressure. ECP is most often performed along with cataract surgery but can be done on an outpatient basis when in the best interest of the patient. The majority of patients having ECP reduce or eliminate their need to take glaucoma medications.
Filtration Surgery
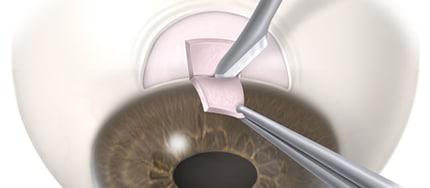
Filtration surgery is performed when medicines and/or laser surgery are unsuccessful in controlling eye pressure. During this microscopic procedure, a new drainage channel is created to allow fluid to drain from the eye.
Minimally Invasive Glaucoma Surgery
Selective Laser Trabeculoplasty (SLT) and Minimally Invasive Glaucoma Surgery (MIGS) are treatments for lowering the eye pressure in patients with open angle glaucoma.
MIGS (minimally invasive glaucoma surgery) is another surgical treatment that is performed to lower the eye pressure in patients with open angle glaucoma. At Central Valley Eye, the main MIGS procedure performed is the placement of a device called the iStent. The iStent is a small metal tube that is inserted through the trabecular meshwork, allowing fluid in the eye to pass through and exit the eye, thus lowering the pressure. Open in place, the iStent is left in the eye for the rest of your life. In most cases, the iStent is offered to patients at the same time as their cataract surgery, when the surgeon is going to be working in the eye. The placement of the iStent adds about 5 minutes to the cataract surgery.
The metal in the iStent is safe for use in an MRI machine and will not set off metal detectors at security. Correct placement of the iStent in the trabecular meshwork makes it impossible to see it with the naked eye, however, your surgeon will be able to confirm its position during clinic visits using special mirrored lenses.
Other MIGS procedures, including goniotomy, supracilliary bypass procedures and ciliary ablation are considered on a case by case basis and will be recommended if your surgeon believes it would be of benefit.
Selective Laser Trabeculoplasty (SLT)
Selective Laser Trabeculoplasty (SLT) and Minimally Invasive Glaucoma Surgery (MIGS) are treatments for lowering the eye pressure in patients with open angle glaucoma.
SLT is laser procedure in which a low energy laser beam is precisely aimed at the trabecular meshwork inside the eye. The trabecular meshwork is the “drain” inside the eye that has stopped working well in patients with open angle glaucoma, resulting in high pressure in the eye. The laser energy causes a very low-grade inflammation in the trabecular meshwork, attracting immune cells to the area to clean up and improve the functioning of the trabecular meshwork. As a result, the outflow through the trabecular meshwork increases and the pressure of the eye goes down.
SLT does not improve the clarity of your vision. However, by lowering the eye pressure in patients with glaucoma, it can prevent vision loss. It may also decrease your reliance on pressure lowering eye drops. The treatment typically takes 5-10 minutes to complete but the entire visit may last 2-3 hours. The pressure lowering effect usually last one to two years. It can be repeated once or twice, however subsequent treatments are usually less effective than the first treatment.
SCHEDULE AN APPOINTMENT
If you would like to learn more about Open Angle Glaucoma call 1-800-244-9907 to make an appointment at Central Valley Eye Medical Group.